Table of Contents
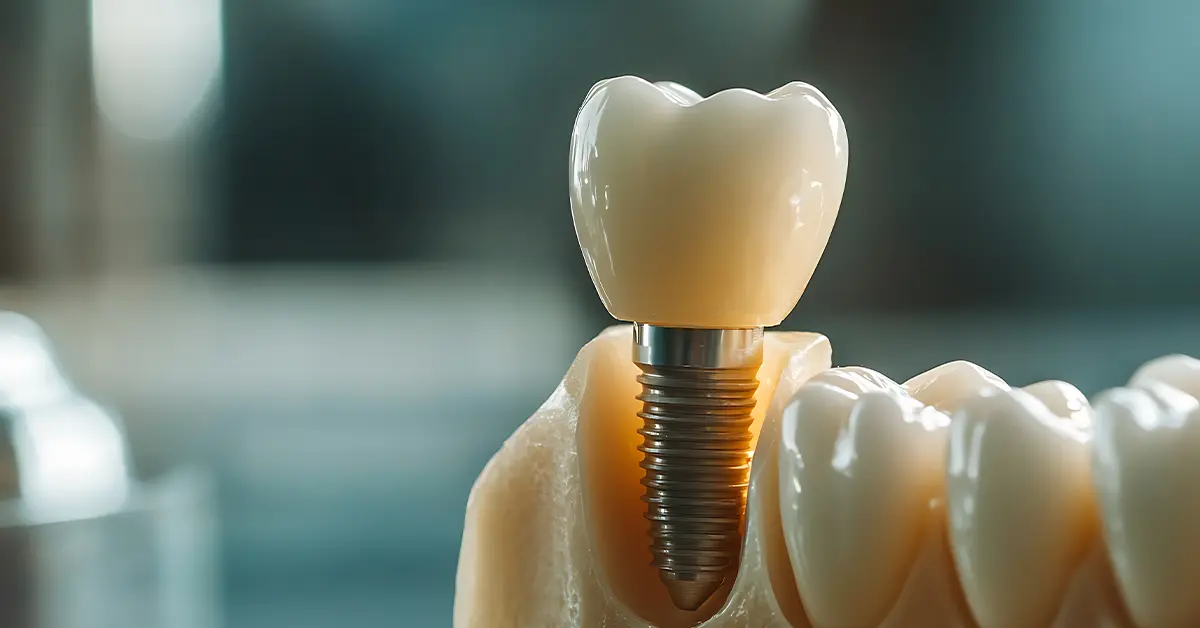
ToggleImplant fall out? If the correct indication, strong bone structure, and regular maintenance are in place, the likelihood is low. However, there is never zero risk. A failed implant application becomes apparent in the first months of healing. If the bone-implant connection is not sufficiently strong, small micro-movements can lead to a chain of problems. If proper care is not taken, the situation worsens when biting force is high and smoking is added to the mix.
Will the implant fall out? In which cases does the risk increase
The answer to the question Will the implant fall out lies in the application and care. If bone volume and density are insufficient or systemic diseases are out of control, the success rate decreases. Smoking has a significant impact. It reduces blood flow, leading to micro-movements. When these conditions occur together, the implant procedure is at risk. Infection also rapidly changes the picture; mucositis in the early stages turns into peri-implantitis if left untreated. As a result, a single mistake leads to a series of problems.

- Acute infection and poor oral hygiene
- Insufficient bone thickness/density, need for grafting
- Uncontrolled diabetes and use of anti-resorptive drugs
- Cigarettes, hookah, nicotine pouches
- Bruxism (teeth grinding) and lack of night guard
- Malocclusion: high crown, unbalanced contact
Will the implant fall out? Early warning signs
Will the implant fall out? For someone experiencing this concern, the most valuable thing is to recognize the signs in time. Falling out is not usually sudden; first, redness in the gums, bleeding when brushing, and bad odor appear. A slight “play” sensation during chewing or loosening of the screw is a warning sign. A decrease in bone level on an X-ray indicates an underlying load/inflammation problem. At this stage, prompt intervention can save the implant.

- Persistent throbbing, especially pain that increases at night
- Redness, swelling, discharge, and a metallic/bad taste
- Bleeding when brushing and sensitivity around the implant
- A feeling of looseness or “clicking” when chewing
- A decrease in bone level on the radiograph
Will the implant fail? Planning and surgical errors
The engineering aspect of the question “Will the implant fail?” is resolved at the planning table. When 3D planning and surgical guides are not used, sinus and nerve distances may be misread. Insufficient primary stability, low torque, and excessive heat production during drilling increase the risk of bone necrosis. An implant that is off-axis transfers forces incorrectly and wears down the bone. Abutment incompatibility increases bacterial load through microleakage.

- Placement without 3D imaging/guide
- Low torque and lack of primary stability
- Inadequate heat control during drilling
- Off-axis placement and incorrect load distribution
- Inappropriate abutment, microleakage, and screw loosening
The effect of care, nutrition, and smoking
An implant can become inflamed like a natural tooth; the difference lies in the connective tissue architecture and bacterial adhesion dynamics. If home care is not regular, plaque toxins rapidly convert to peri-implant mucositis. Soft foods and gentle cleaning in the first weeks support healing. Alcohol-containing mouthwashes can irritate sensitive tissues; abrasive toothpastes also strain the gums. When smoking is stopped, healing accelerates significantly and long-term success increases.

- Daily care: soft brush + interdental brush/floss + water jet
- Product selection: low-abrasive toothpaste, alcohol-free mouthwashes
- Nutrition: soft foods for 2–4 weeks; avoid extreme hot/cold
- Habits: quit smoking/nicotine or at least take a break around the time of surgery
- Check-ups: 1, 3, 6 months; then yearly clinical + x-ray
Revision, salvage, and cost: What is done, and when?
Not every adjustment means the implant will be removed; the correct differential diagnosis makes a big difference. Simple torque adjustment and occlusion adjustment may be sufficient for screw loosening. Professional cleaning and antiseptic protocol often yield results in mucositis. If peri-implantitis has progressed, debridement and, if necessary, regenerative surgery (graft/membrane) come into play. Even in implants that need to be removed, success can be achieved with re-planning after the correct healing period.
- Screw loosening: retorquing + bite height adjustment
- Peri-implant mucositis: professional care, local antiseptic protocol
- Peri-implantitis: debridement, bone regeneration if necessary
- Failed implant: atraumatic removal → healing → re-implantation
- Cost: minor revisions are more economical; advanced grafting increases cost
Check out our social media to see the successful results.
Frequently Asked Questions
My implant is slightly loose; will it fall out immediately?
Generally no. Depending on the cause, stability can be regained with screw torque, bite adjustment, and hygiene treatments.
I smoke; how much does this affect my chances of success?
It significantly decreases them. Quitting is best; at least take a definite break before and after surgery.
I have no pain but there is an odor; is this dangerous?
Yes. It could be a sign of silently progressing inflammation. A clinical evaluation and X-ray are required.
Can a fallen implant be replaced?
In most cases, yes. After infection control and bone healing, the implant is reinserted with the correct axis and load plan.