Table of Contents
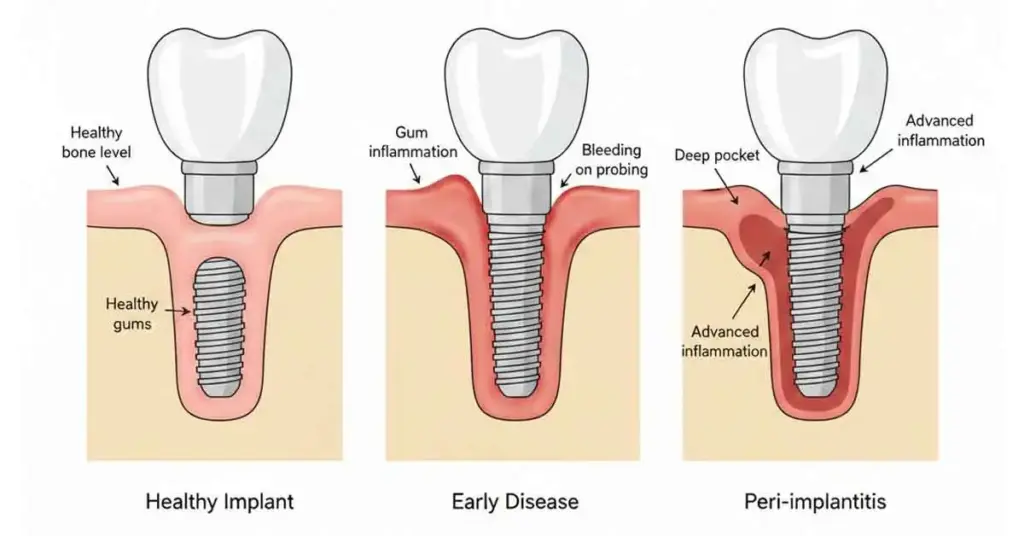
TogglePeri-implantitis is the inflammation of the bone and gum tissue surrounding the implant. In other words, it is not the implant itself that has a problem, but rather the living tissues that support it. The question “What is peri-implantitis?” actually means: Why do the supporting tissues around the implant become red, swollen, and bleed, leading to bone loss over time? If left untreated, this condition can lead to loosening and eventual loss of the implant. Therefore, early diagnosis is crucial. In this article, we discuss the symptoms, causes, treatment options, and prevention methods of peri-implantitis in a detailed yet understandable manner. This provides a clear roadmap for both patients and individuals with implants.
What is Peri-Implantitis? What are its Symptoms?
Peri-implantitis is a disease characterized by inflammation of the gums around the implant and underlying bone loss. When we ask, “What is peri-implantitis?”, we are actually describing a more advanced condition that goes beyond gum inflammation and affects bone tissue. We may see redness, swelling, bleeding, sensitivity, and sometimes bad odor around the implant. Some patients experience mild discomfort, while others feel significant pain when chewing. As the process progresses, we may see pockets around the implant and notice bone loss on x-rays. Patients usually visit the clinic complaining of bleeding while brushing, a feeling of fullness in the gums, and sometimes slight mobility in the implant area.
• Redness and swelling around the implant
• Bleeding while brushing or eating
• Sensitivity or pain around the implant
• Bad breath or unpleasant taste
• Receding gums and exposure of the implant surface
• In advanced cases, a feeling of loosening in the implant
GET INFORMATION FAST!
What Causes Peri-Implantitis? What Are the Risk Factors?
Peri-implantitis is most often caused by a combination of factors rather than a single cause. The most common cause we see is insufficient daily cleaning around the implant. As plaque and bacteria accumulate, mucositis develops around the implant, which progresses to peri-implantitis if left untreated. Smoking, diabetes, weakened immune system, uncontrolled systemic diseases, and failure to attend regular check-ups significantly increase the risk. Improperly planned implant positioning, insufficient bone volume, poorly fitting prostheses, and excessive chewing load also contribute to the condition. When we look at it, the answer to the question “What is peri-implantitis?” is not just infection; it is a process involving hygiene, habits, and quality of planning.

• Inadequate oral and implant site hygiene
• Smoking and nicotine addiction
• Uncontrolled diabetes and chronic systemic diseases
• Failure to attend regular dental check-ups
• Improperly planned implant placement
• Prosthesis design that makes cleaning difficult
• Excessive chewing forces and nighttime clenching (bruxism)
How is Peri-Implantitis Treated?
The goal of peri-implantitis treatment is to control inflammation and stop bone loss. The first step is always a thorough clinical and radiographic evaluation. Plaque and calculus around the implant are removed, and the surfaces are thoroughly cleaned using special instruments and sometimes laser systems. In the early stages, we can achieve good results with mechanical cleaning and antiseptic solutions alone. In moderate and advanced cases, we add local or systemic antibiotics. In cases where bone loss is significant, surgical treatment, bone grafting, and membrane applications come into play. In some severe cases, implant removal becomes the healthiest option. We create a treatment plan individually for each patient.
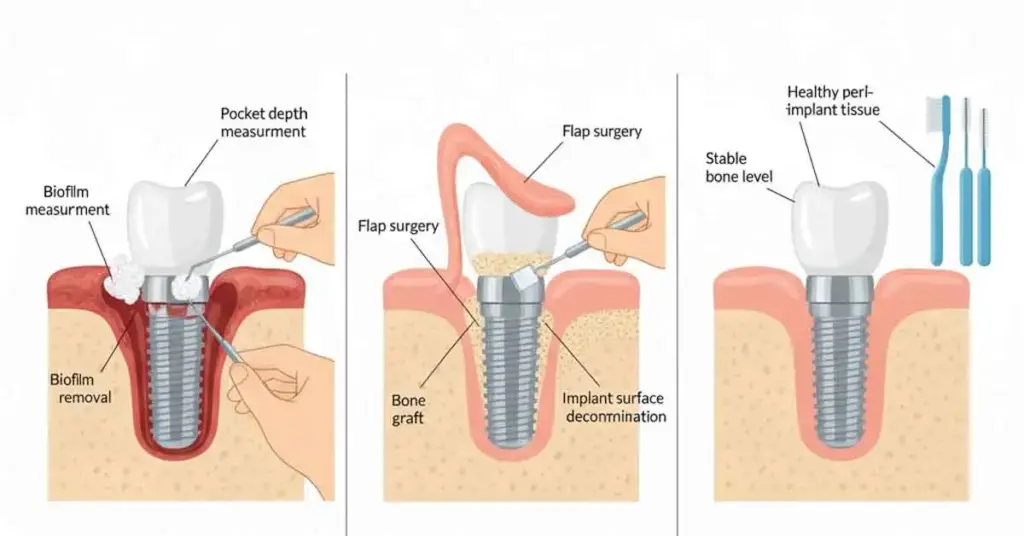
• Detailed clinical and radiographic evaluation
• Professional cleaning around the implant
• Antiseptic mouthwashes and gel applications
• Local or systemic antibiotics when necessary
• Surgical cleaning, bone grafting, and membrane use
• Removal of the implant in irreversible cases
• Frequent follow-up and maintenance program after treatment
What Can We Do to Prevent Peri-Implantitis?
Peri-implantitis is a problem that can be largely prevented with proper care and regular check-ups. From day one, personalized care training is important for patients who have implants. The area around the implant must be carefully cleaned every day with a soft-bristled brush, interdental brush, dental floss or superfloss, and a mouthwash recommended by the dentist. If you smoke, reducing or quitting will positively affect both the healing process and long-term success. When we look at it, the most protective answer to the question “What is peri-implantitis?” is regular professional care and a disciplined routine at home. At least two check-up visits per year allow us to catch small problems before they become big ones.

• Daily regular and proper brushing habit
• Detailed cleaning with an interdental brush and implant floss
• Use of antiseptic mouthwash at intervals recommended by the dentist
• Reducing or completely quitting smoking
• Regular monitoring of systemic diseases
• Professional care and check-up appointments 2–3 times a year
• Regular monitoring of the fit and load distribution of prostheses
Peri-Implantitis – Frequently Asked Questions (FAQ)
Can peri-implantitis be detected early on?
Peri-implantitis often presents early signs such as gum redness, mild swelling, and bleeding during brushing. When these symptoms appear around the implant, coming in for a checkup without delay allows us to stop the disease in its early stages.
What happens if peri-implantitis is not treated?
If left untreated, the inflammation slowly erodes the bone around the implant. Over time, the implant loses support, begins to loosen, and may eventually need to be removed. Pain, infection, and aesthetic loss may also occur during this process.
Does peri-implantitis always result in implant loss?
No. In cases caught in the early and middle stages, we can keep the implant in the mouth for many years with proper treatment and regular follow-up. If bone loss is very advanced and the implant has lost a significant amount of support, then we consider extraction.
Is it possible to treat peri-implantitis at home?
Good oral hygiene at home, using antiseptic mouthwash, and quitting smoking support the process, but they are not considered treatment on their own. Peri-implantitis is a condition that requires professional intervention. Therefore, instead of waiting for it to “go away,” you should visit the clinic.
What is the difference between peri-implantitis and mucositis around the implant?
In mucositis around the implant, there is only gum inflammation; the bone is not affected. In peri-implantitis, both the gum and bone tissue are involved in the process. Therefore, peri-implantitis is considered more serious, and the treatment approach is more comprehensive.
How long does it take to treat peri-implantitis?
The duration varies depending on the severity of the disease. In some cases, a few sessions of professional cleaning and monitoring may be sufficient, while in advanced cases, surgical procedures and a longer follow-up period may be necessary. The important thing is how early we start treatment.
Aslı Yılmaz
Dentist – Her education at Istanbul University Faculty of Dentistry. Specialist in dental treatments.

